For decades, Body Mass Index (BMI) has been the standard tool doctors use to decide if someone is underweight, overweight, or obese. It’s quick, cheap, and widely used—but here’s the catch: it may not tell the full story about your health.
Many experts now argue that BMI is outdated, overly simplistic, and even misleading when used to judge individuals. So, how accurate is it really—and what are the better alternatives?
Table of Contents
🔹 What Exactly Is BMI?

BMI stands for Body Mass Index, a formula created back in 1832 by Belgian mathematician Lambert Adolphe Jacques Quetelet.
His goal? To give governments a way to quickly assess whether populations were overweight or obese—not to measure individual health.
The formula is simple:
- Metric: BMI = weight (kg) / height (m²)
- Imperial: BMI = (weight (lbs) / height (in²)) × 703
Your number is then compared to categories:
| BMI Range | Classification | Risk of Poor Health |
| Below 18.5 | Underweight | High |
| 18.5 – 24.9 | Normal weight | Low |
| 25.0 – 29.9 | Overweight | Low to Moderate |
| 30.0 – 34.9 | Obese Class I (Moderately Obese) | High |
| 35.0 – 39.9 | Obese Class II (Severely Obese) | Very High |
| 40.0 or greater | Obese Class III (Extremely Obese) | Extremely High |
Some countries even tweak BMI cut-offs. For example, Asian populations tend to face higher health risks at lower BMIs, so different ranges are used.
But while BMI is easy to calculate, it doesn’t consider age, sex, muscle, fat distribution, or genetics—all of which can drastically change what “healthy” really means.
🔹 Is BMI a Reliable Indicator of Health?
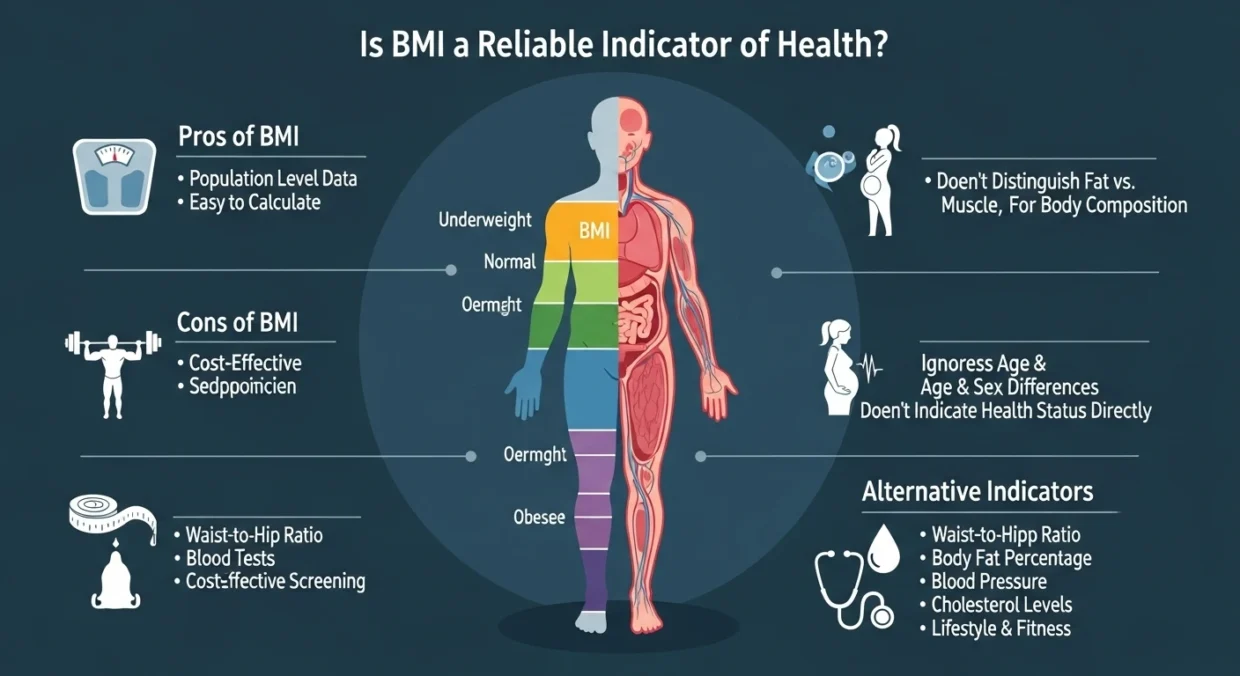
Despite its flaws, research does show strong links between extreme BMIs and health risks.
- People with a BMI below 18.5 (underweight) or above 30 (obese) face a higher chance of chronic disease and even early death.
- A 2017 study of 103,000 deaths found that people with obesity had up to 2.7 times greater risk of dying compared to those in the normal range.
- Other research shows obesity is linked to heart disease, type 2 diabetes, fatty liver disease, mobility issues, and kidney problems.
Even a 5–10% reduction in BMI has been shown to lower risks of metabolic syndrome, diabetes, and heart disease.
So, BMI is a useful population-level snapshot—but not a reliable tool on its own for judging an individual’s health.
🔹 The Hidden Downsides of BMI
1. It Ignores Other Health Factors
BMI doesn’t consider cholesterol, blood pressure, blood sugar, or inflammation. It also doesn’t distinguish between fat, muscle, or bone.
2. Muscle vs. Fat Confusion
Because muscle is heavier than fat, athletes and bodybuilders are often mislabeled as “overweight” or “obese” even when they’re very lean.
3. Fat Distribution Matters More
Where your body stores fat is often more important than how much you have.
- Apple-shaped bodies (fat around the belly) have higher risks.
- Pear-shaped bodies (fat in hips/thighs) may actually have protective benefits.
4. Weight Bias in Healthcare
Some doctors rely too heavily on BMI, which can lead to misdiagnoses or delayed treatment. Patients with higher BMIs often report negative healthcare experiences, making them less likely to seek regular checkups.
5. It Doesn’t Work Equally Across Populations
- Asian populations face higher disease risks at lower BMIs, which is why WHO created Asian-specific BMI cut-offs.
- Black populations often have more muscle and less fat at a given BMI, meaning they may be misclassified as overweight even when they’re healthy.
- Cultural differences around body size also affect how health should be understood across groups.
Read More:Is BMI Failing Black Women? The Hidden Truth About This Popular Health Measure
🔹 Better Alternatives to BMI
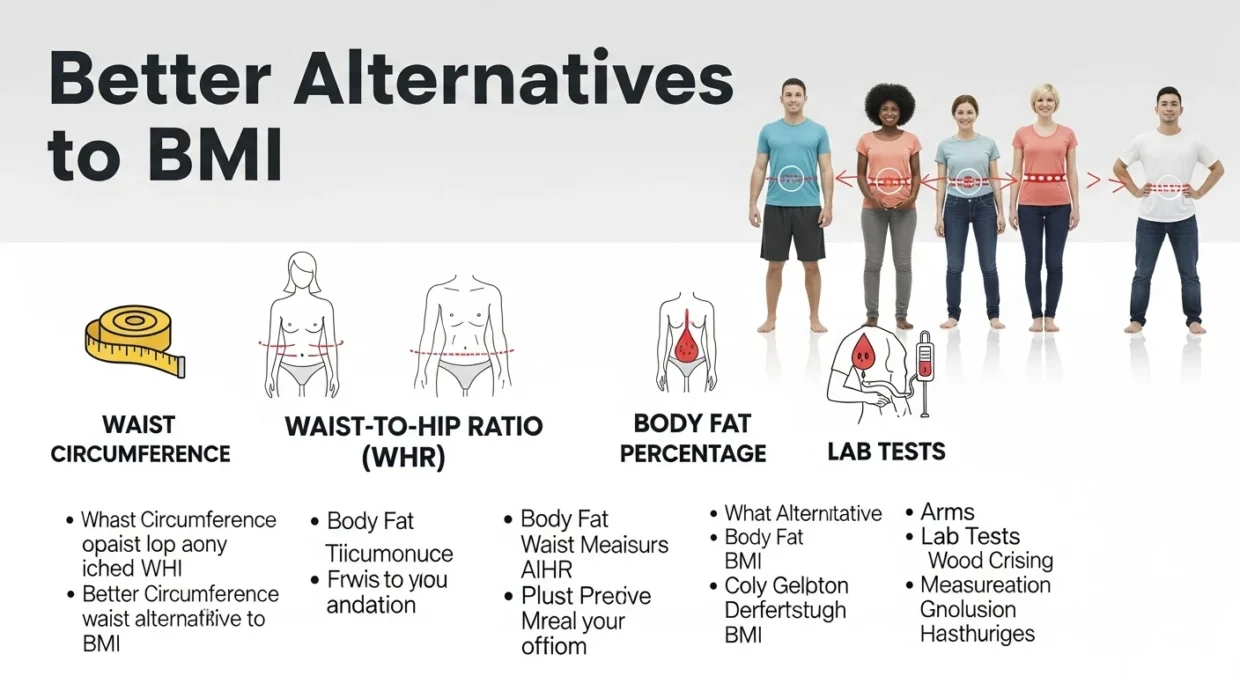
While BMI isn’t going away soon (it’s simple, cheap, and widely available), there are better ways to measure health:
✅ Waist Circumference
- A waist larger than 35 inches in women or 40 inches in men suggests higher risk.
- Easy to measure but doesn’t account for body type.
✅ Waist-to-Hip Ratio (WHR)
- High ratios mean more belly fat and higher health risks.
- Low ratios (more hip fat) are linked to better outcomes.
- Quick and simple, but still ignores muscle and bone mass.
✅ Body Fat Percentage
- Distinguishes fat from lean mass, making it more accurate than BMI.
- Affordable methods (like smart scales or skinfold tests) aren’t very precise, while accurate tools (like DXA scans) are expensive.
✅ Lab Tests
- Blood pressure, cholesterol, blood sugar, and inflammation levels give a much clearer picture of overall health.
- More reliable, but usually require medical visits and context from multiple tests.
🔹 The Bottom Line
BMI is easy to calculate but easy to misuse. While it can highlight population health trends and flag extreme risks, it doesn’t tell the full story of an individual’s health.
It ignores muscle, fat distribution, ethnicity, age, lifestyle, and mental health—and relying on it alone can even fuel weight stigma in healthcare.
The takeaway:
- BMI can be a starting point, not the final word.
- For a real health picture, pair it with waist circumference, body fat analysis, lab tests, and lifestyle assessments.
- Most importantly, health should be defined individually—not by a single number.